There are numerous articles and many more videos of people showing you how to help your sciatica nerve pain. Many of these articles briefly glance over the anatomy. The problem is that anatomy and functionality is the most important part in ridding your sciatica nerve pain.
As a Spine and Sports Medicine Specialist in Long Beach, California, we have helped 1000’s of people walk, run, lift, and resume their sport after dealing with sciatica. You can get better too.
Do you know if you have sciatica or something that mimics sciatica?
That is the first clinical riddle that we must answer when we first try to help a client dealing with nerve pain to their leg.
Basic Anatomy 101: Sciatic Nerve
Your sciatic nerve is a combination of your tibial and common fibular nerve. At this junction, the two bundle of nerves connect to your four hamstring muscles and adductor magnus muscles. Your hamstring muscles consist of your semimembranosus, semitendinosus, long head bicep femoris, and short head bicep femoris muscles.
If you have tight hamstrings muscles that is not resolving after stretching for 2-3 weeks, then you will benefit from this article. If you reside in Long Beach or the neighboring Los Angeles cities and you need immediate sciatic pain assistance click on the button below. We can help you if you prefer to speak to a Spine and Nerve pain Specialist immediately.
We are going to start our anatomy lesson beginning from the top of the nerve anatomy to the bottom.
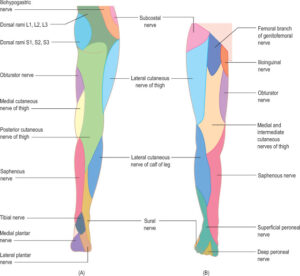
The two nerve bundles (tibial and fibular nerve) stems from the front branches (ventral rami) of spinal nerves L4-5, and S1-S3.
As a nerve crosses a joint, bone, muscle, ligament, and/or tendon, there is a chance that the nerve can be impacted by that structure OR that structure can impact the sciatica nerve.
Here is a quick example to explain a very important point we just wrote.
The L4 or L5 nerve root can be dysfunctional based on how tight or health of your hip flexor muscles. This is a “nerve being impacted by a structure” example. If you have poor pelvis posture that places your hip flexor muscles into a state of tightness or stiffness, you are placing your spinal nerve root into tension too.
The situation can be said that your tight hip flexor muscles can be due to a L4 or L5 nerve root dysfunction.
If you have been told to stretch your hip flexor muscles and it has not been resolved after 2-4 weeks, then you may have a L4 or L5 spinal nerve root dysfunction. Your hip flexor muscles are reacting to the nerve problem.
We will be writing more and more examples of this exact idea, because it could be the missing link in your sciatica nerve pain rehabilitation.
Let us get back to the anatomy of the nerve itself.
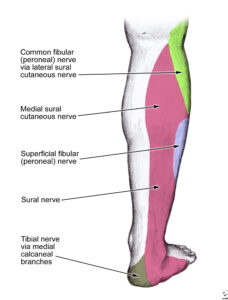
As L4-S3 spinal nerves converge into the sciatic nerve around the posterior (back of the) hip region, the sciatic nerve splits to the tibial and fibular nerve just above the back of your knee. The tibial nerve generally supply your back and inner leg. Your fibular nerve supply your back and outer leg.
The tibial nerve splits into your plantar nerve to supply your foot.
Your fibular nerve splits into the Sural nerve to supply your outer shin and foot region. The anatomy of the lower leg nerve branches is why you maybe experiencing leg pain down to your calves, even though the sciatic nerve ends much higher.
As you can see how the path of the nerves is far from straight and simple. You have nerves that originate at each spinal level to twist and turn like the many freeways that we drive on.
Nerves function becomes impacted when the nerve gets compressed or stretched abruptly. The more common scenerio where the sciatic nerve gets injured is having a compression force near the spine and sacrum.
The possible musculoskeletal sources of sciatica pain include having a disc herniation, bone spur, ligament thickening, or fascial tissue restriction along the pathway of the nerve. This compression idea is what many believe and get diagnosed with a “pinched” nerve. There is more to sciatica than you may know.
If the origin of sciatica is only mechanically explained, why are there millions of people with bad back surgery?
The surgeons eliminate the compression to the nerve, but the people are still slowed down with the severe nerve pain.
Many tend to feel extreme pain very early on in their sciatica episode because there is a chemical tissue irritation response. As inflammation is broad, multiple tissues around the nerves are symptomatic. This is why many feel more pain the first three to six months of having sciatica. The pain is broad and common to feel pain all over the back, hip, and/or leg.
As inflammation eases up with smart movement, icing, and hydration, many people feel a reduction of their sciatica nerve pain. An epidural focuses on addressing the chemical portion of having sciatica.
Nerve tissues hates to bathe in the water called inflammation.
As you feel better or have a low grade form of sciatica, you may have no tight or painful leg pain without lower back pain. This situation is one of the hardest for patients to understand. The reason for the leg pain without the lower back pain can be sourced to a terminology called nerve entrapment.
As a Spine specialist that have helped many chronic sciatica sufferers, we hope to shed more light on reasons many doctors and surgeons do not acknowledge. Your pain is not always where you feel them. Nerves are followed in long pathways.
Think of your nerves as plumbing pipes in your house. Your toilet is clogged. The problem is not your toilet. The problem can be at the main sewer line, which is far from the toilet.
Your brain and spinal cord can be thought of as extension of your sciatic nerve.
As your nerves connect to your brain and spinal cord, you have to consider the impact of your sciatic nerve as a part of the nervous system.
An unhealthy nervous system, or nervous system that has been through trauma or past injuries can be a source of making the sciatica more vulnerable to injury. A classic example that we see and manage with great success is when someone with present day of chronic sciatica and had a past history of whiplash or concussion.
A great metaphor that many people understand is to imagine your brain, spinal cord, and the sciatic nerve as a rubber exercise tube. A rubber tube is best when it can stretch and twist to its maximum capacity, but still able to recoil back to its original position.
If you take the rubber exercise sport tube and stiffen the rubber to be of a dried rubber, the exercise tube cannot stretch out as well. This idea demonstrates how the other end of the tube has to over stretch if the tube is to reach the same limit as if the whole tube is elastic.
Many people who have dealt with a concussion or been in a car accident resolve to resume their normal daily tasks. The problem is when there was no professional rehabilitation or Physical Therapy care, and people stress their body to the same limit.
If you walk, run, push, pull, lift, and/or be active in any forms with your hips and legs, you are potentially tugging on your Exercise Sports Tube more than what it likes.
It is wise to keep a reminder that nerves likes to be stretch, but not over stretched.
If there is post-trauma side effects that is resulting in fascial or connective tissue tension to the cranium and neck region, you have to release that tension with a Sports Physical Therapist that specializes in Spine and Nerve injuries.
As a Sports Medicine Physical Therapist, we have our fair share of helping athletes who had a history of concussion-like football, rugby, and soccer players get back to their sports. Our hands-on manipulation to the neck and cranium specialty has been instrumental as many medical practitioners forget that the sciatic nerve is part of the nervous system.
You manage the system, and not the individual part, to ensure the parts are working well!
The common scenario of “sharp, shooting, pain down the leg” is primarily driven by mechanical stress to the spinal nerve, sciatic nerve, and/or it branches. The chemical inflammation can amplify and broaden the area of pain.
.
The idea of a mechanical fascial entrapment means that the nerve cannot slide, twist, and move freely within the body’s fascia framework. Fascia is a connective tissue system that mirrors that image of a spider web.
A spider web provides structure and support. The design allows it to be strong. Your fascia surrounds all tissues within your body. Your nerves, arteries, veins, and lymphatic vessels travel in between the fascia’s spider web gaps.
If the fascial gaps become fibrotic and fuzzy, the area around this fascia will not have the best circulation, nutrition exchange, waste elimination, and/or nerve communication. When the fascia impacts the nerves and the nutrients that keeps tissues from being at peak health, you can get sensory changes to the area that the nerve supplies.
.
There are situations where you will feel pain to your calves, but the root source is a fascial entrapment of the sciatic nerve along the pathway down to the back of your leg or spine.
As we used the example of having “psuedo-calf pain”, you can have localized pain to the muscle or joint tissues. If the incident is recent in nature, the sensitive muscle or joint tissues is of fascial-neuro origin.
As nerve impacts the function of your muscles and subsequent joint system, the side effects of having an altered nerve input is painful muscle tissue. Painful muscle tissue can still produce strength. This is similar to muscle tendinitis or tendinopathy scenario. This fools many medical practitioners, including surgeons and orthopedists.
Anatomy 102: Joint and muscle perspective.
Your L4 to S3 spinal nerve root is located directly in front of your sacrum and ilium bone. The two bones connect to make your sacroiliac joint. Your sacroiliac joint’s role is to help transmit the kinetic chain forces of walking, running, and playing sports up and down your body.
You can see how important your Sacroiliac joint can be. Your sacroiliac joint is the foundation for your hips and legs to swing from. If you run, your leg should swing back and forth evenly, like a pendulum. You can see that your spinal vertebrae stacks on your sacrum bone as its foundational base of support.
If your nerves cross over a joint, the mechanics and integrity of the joint have a crucial role in that nerve’s health. Motion is lotion. If you do not have adequate range of motion to your sacroiliac joint, then the spinal nerves, nerve plexus, and the convergence of the sciatic nerve becomes impaired.
.
There will less nutrient exchange, circulation, and stagnant capacity to rid of toxic waste products to the nerves around the sacroiliac joint when you have a stiff spine.
A physical therapist skilled in Orthopedic and Spine will be able to detect if you have spinal stiffness. You do not need to feel stiffness in your lower back area. When we perform a local Spine Accessory testing, many agree and understand how their local spine stiffness is impacting their sciatic nerve.
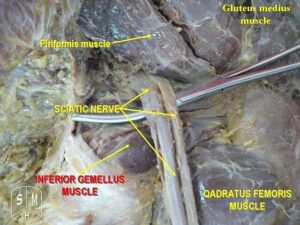
We will move down to the n ext important tissues that have a big role in sciatic nerve pain. Your Piriformis muscle can a source of placing nerve stress. There is a small percentage of people where the sciatic nerve courses directly between the piriformis muscle.
When you contract or place pressure directly to the piriformis muscle, you will feel the deep gluteal pain. You may feel the pain that has been traveling down your leg.
.
You can see how the sciatic nerve is impacted by the hip joint. The sciatic nerve runs to the posterior hip. A healthy hip joint spins around the acetabulum socket. When you contract the muscles to the front of the hip joint, like the hip flexors or adductor muscle group, you get a minor shift of the hip forward. When you contract your gluteal muscles, located to the back of your hip joint, you get a small shifting of your hip joint back.
All of these minor hip joint shifting is not a problem. The trouble arises when you cannot control the shifting that occurs. If your hip joint is moving excessively, your sciatic nerve can take some of this neighboring stress.
The stress is in the form of micro stress. The tricky part is that this takes years and is undetected by you. The early warning signs of a hip or sacroiliac joint that you cannot control are included in the list below.
- tight lower back muscles that reoccurs shortly after stretching
- tight hamstring muscles that reoccurs shortly after stretching
- hip makes popping noise when you move at times
- tight hip flexors muscles
- front of the knee pain
- ankles that feel tight
- gripping with your toes often
You can see that the effects of poor hip muscle control has an effect down the kinetic chain.
You can make the conclusion that micro and macro stress to the back of the knee and ankle can impact the sensitivity to the nervous system nearby. Nerve related stress can have an upstream and downstream impact to the associated nerve fibers.
.
An example is how the lower end nerve branches, like the lateral or medial plantar nerve, can get twisted during an ankle ligament sprain. The neural tissues from the macro trauma can impact upstream to the sciatic nerve within the posterior thigh or sacroiliac joint region.
If you suffered from an Anterior cruciate ligament sprain, you can have nerve stress to the tibial nerve. The tibial nerve can have a downstream impact to the plantar nerve or laterally to the sural nerve. The upstream impact will be to the lumbar or sacral plexus, spinal nerve root L4, L5, or S1, and sciatic nerve.
We will continue more with Part 2 of this article. Part 2 will go over tissues that can mimic sciatic nerve pain and tips on how to know if you have sciatic nerve pain or something else.

