We have a special treat for you readers in this article. It comes from the passionate and generous teachings of Ron Hruska, the founder of Postural Restoration Institute. Their teachings and clinical practices can be seen in many Sports Medicine and Performance Specialist clinics and gyms. They are becoming the cutting edge of integrating sound holistic biomechanics into performance. Due to the COVID-19 pandemic, Ron Hruska is educating on the lung’s impact on posture and strength. He picks his favorite go-to exercises based on the week’s topic.
You will get a sense of how simple movement can have a profound impact from a kinetic movement chain and physiologic-movement perspective. We found it exciting to learn how each week’s webinar builds on top of each other to round out to one big concept. The lungs are the root of many peoples problems!
This article is our interpretation and summary of Postural Restoration Institute’s concepts. If you are interested we highly suggest you click on this link HERE to watch and learn first hand.
Introduction Topic on Compliance (click to watch the video)
This video brings on the difference of compliance and pressure. Compliance implies the ability to conform and be manipulated. Pressure is the resultant force that comes with movement. The two need to be understood and applied in different ratios so you can be control of the environment and situation for optimal health.
Compliance helps us to not get injured! The more we can absorb and release tension because our tissues are elastic and pliable, our tissues are not holding tension over a prolonged time. We need to relax and this takes energy when we are more on the “pressure” side of the equation.
If you need to be produce maximal strength, you need pressure and less compliance. You do not want a pliable lower back and hips, as much as you need control force to move heavy object. If you can harness focused pressure while keeping compliance, you have the winning edge.
This can be seen in Michael Jordan’s ability to manipulate a basketball and dominate his foes.
Compliance and pressure needs to cycle to bring a rhythmic and necessary compression and decompression pumping effect. Numerous systems in our body is regulated through a pumping cycle, such as a heart beat or a gut motility cycle. Our ability to move requires a systemic and holistic cycle of compliance and pressure, which is maintained by two factors listed below.
- Respiration efficiency of inhalation and exhalation.
- The visceral organ ability to move independently of the musculoskeletal encasement during movement such as the cycle of locomotion.
The more our visceral organs move independent of each other and the neighboring tissues, the less pressure is needed to move our bodies. There was a fascinating reference to an article on how a liver transplant can be kept healthy and viable for 2-3 more hours when compliance is maintained. The liver tissue becomes less “pressured”.
There is another reference to an article on how laying on your stomach can bring more compliance cycle to COVID-19 patients. There is more perfusion and ventilation to the lungs as laying on your stomach will replace the pressure that your body will need to produce. Your diaphragm will have to work harder to bring rhythm back. Your body can relax and be compliant again. Again, the more compliant you are the more you can ride a virus load.
As you read the rest of the article, be mindful of compliance and pressure regulation to improve movement and ease pain.
Week 1 – Pleura, Lung & Chest Wall Relationships to Physiological and Physical Mechanics (click to watch the entire video)
The first week starts with a quick overview of the lung anatomy and the nuances that impact each of the individual lungs. The main point is that ventilation (air exchange) and perfusion (fluid exchange within the capillaries) of the lungs need to be in contact. If that is disrupted, then the gas exchange will be changed. This is will tie into Week 4’s webinar. The lung is a very efficient machine that runs on minimal energy because it is the gas exchange and airflow that causes the lung to function. The lung is pumped by the diaphragm muscle that is underneath the lungs.
The lung is surrounded by the rib cage (chest wall) and its associated pleura. The lung is encased by the visceral pleura. The inner chest wall is surrounded by the parietal pleura. In between the two pleurae is fluid that helps allow it to move, slide, and glide independent of each other. This is important as local lesions can cause ketchup-like fluid consistency that will impact your breathing and rib mechanics.
The fluid and space (intrapleural pressure) result in a negative pressure of 756 mm Hg (-4 mm Hg difference) that keeps the lungs inflated. This produces a suction pressure between the rib cage and the lungs. Flow moves from high to low. The lung pressure, or atmospheric pressure and intra-alveolar pressure, is higher at 760 mm Hg. Remember that flow goes from high to low.
If the atmospheric pressure is lower because of altitude or your alveolar pressure increases above normal 760 mm Hg, you will have a hard time getting air into your lungs. The same goes for the opposite pattern. Airflow into the lung when the alveolar pressure is lower than atmospheric pressure. The respiratory muscles will contract to open up the lungs. When you get air into your lungs, the flow of gas opens up the lungs with the pleural cavity suctioning the lungs to open too. When you get a description of this pressure gradient, the loss of suction will result in a collapsed lung.

Exhale can be said of the opposite pattern happening. The intercostals muscle contracts to shift the alveolar and atmospheric pressure gradient.
The right lung has three lobes, which makes is larger, wider, and shorter. The right lung is divided into horizontal and oblique fissures. Your right 4th and 5th ribs is a good area to find the horizontal fissure. Your oblique fissure comes off of the horizontal fissure to orient diagonally from your right shoulder to your left hip.
The left side rib cage is more crowded with the heart and esophagus, so the left lung is smaller, longer, and narrower with 2 lobes. Many are familiar with the need for the lungs to deflate and inflate, but the lungs and rib cage help to absorb shock, provide leverage for stable movement, and moves in recoil and coil-like manner.
If you imagine the twirl and counter-twirl of a washing machine. That is the two pleurae movements upon each other.
Our webinar ends with the importance of re-balancing the three zones of lung perfusion. If you divide the lungs into thirds, zone 1 tends to have more ventilation than perfusion (air over fluid exchange).
Zone 2 has a 1:1 ratio of perfusion to ventilation.
Zone 3 will have more perfusion more than ventilation (more fluid than oxygen).
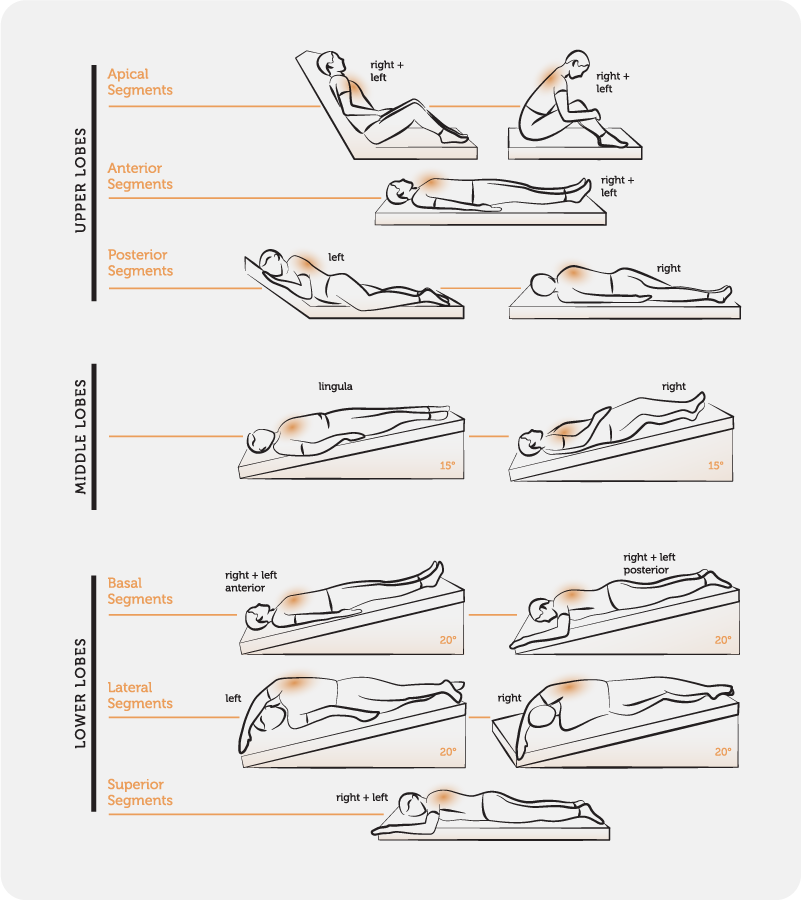
Positions and postural habits can drive the zone perfusion to ventilation ratio. Gravity assists in exchange for perfusion and ventilation matters. An example is that when you lay on your right side, your right lung will get more gas exchange. It gets more gravity assistance. When you are upright and walking, your zone 3, or bottom lungs, naturally get more gas exchange.
Our arms and legs movement and ability to sense the environment will encourage the body-lung axis to maintain healthy ventilation to perfusion ratio. I bolded the word sense to reiterate that if we cannot feel the ground or through our hands, we would have a harder time to breath. This is seen in the diabetic neuropathic patient. You see this when you briefly lose your eyesight. You go into shallow breathing. This emphasizes the importance of swinging your arms just as far as your legs when you walk, skip, and move.
The take-home message is that there is a typical pattern of Right anterior apical (top) and left posterior lower lung restriction.
The solution is to use positions to help drain and improve flow. When you are in supine, your lungs have the biggest ability to move (excursion), but you lose lung volume. When you lay on your LEFT side, the lower chest gains more movement but less volume (stability). Your RIGHT upper chest (apical lung) will get more expansion.
Week 2 – The Roots of Lung Function
The goal of this week’s webinar is to emphasize the importance and positioning of the central airway (trachea and hilus), providing compression to the lung’s dead space during inhalation, and how-to repositioning the chest wall.
The hilus lies in front of T5-7 segments, or bottom third of the shoulder blades.
The mediastinum is the cavity that houses the heart, thymus gland, esophagus, and trachea. For a cool video of your organs in action click on the picture.

The trachea lengthens with these movements.
- Extends neck. (trachea moves backwards into the chest wall).
- Swallows. (trachea stretches upward).
- Inspire. (trachea stretches down into the rib cage.
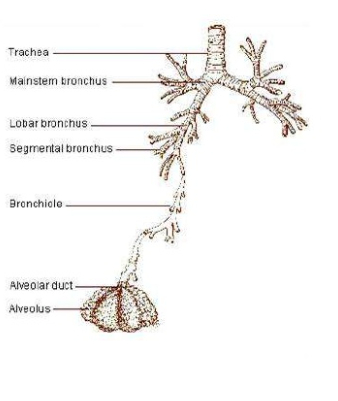
As you can see the bronchial tubes differ from left to right. The right side favors gravity and flow of air. The left bronchii bends more at a 45-50 degrees.
Understanding this will help us aim in re balancing and addressing the typical pattern of restriction of right front apical and left posterior lower lungs. When we position the trachea, bronchi, and root of the lungs, we help open up the tracheobronchial tree AND decrease the fluid accumulation in this possible lung dead space (alveolar ducts and sacs).
What is lung dead space? It is the air that is inhale and not put to use. How can this happen?
- You do not push it out because of hypocapnia (see week 4 webinar).
- There is fluid accumulation and less perfusion in an area, which limits ventilation.
- There is an inability of the alveolar walls to conform and play a part in expelling the air out.
We all have lung dead space to help us trap debris, make mucous to expel, and such. The ratio is 1/3 of every resting breath we take.
Unfortunately, modern society impacts rib cage and lung health so have trapped dead space. This week gave us suggestions to realign the central respiratory connections and to ventilate (more air) into the alveolar dead space. In the COVID-19 times with the fatal symptom of Acute Respiratory Distress Syndrome (ARDS), you get too much fluid building up in the alveoli.
Again, the part of the lung that needs to move the most is the left posterior basal lung. The lung is divided into sections to allow us to move 3-dimensional, but the 3-dimensional movement helps to not allow the lungs to be filled with dead space or fluid buildup to occur.
The key to turning these dead spaces into “live” spaces is to get into various postural positions and to move your limbs often and in many different directions. The rib cage is designed to twist, compress, and lengthen. You can think of an accordion instrument. This will help us to get into small tight spaces and reach for far places, but in doing so, your lungs becomes “alive”.
The suggested exercise for this week is the “Standing supported left glute push”. When you push into the table with a firmly planted foot, you naturally open up the airway to allow the lungs to have the 1:1 perfusion to ventilation ratio. The push will naturally position the tongue and mouth to shift the pressure to close the oral-esophageal pathway. The pharynx and larynx (to the trachea by the tongue) will bring form closure so the abdominals and diaphragm will do most of the work. This will help move any stagnation from the lower lungs.
THERE ARE OTHER POSTURAL DRAINAGE POSITIONS TO GET MORE AIR FLOW.
Week 3 – Balancing Pleura Cavity Negative Pressure Through Ground Pressure.
The right lung has the football-sized liver underneath it, which provides the right lung the stability that the left lung does not have. The anatomical positioning of the right lung tends to make it more vulnerable to being restricted. This idea implies that the right lung does not expand well. Our modern-day liver is usually overworked and becomes limited in its motility and mobility, thus facilitating a restricted right flank pattern.
The left lung is more mobile and expressive than the right lung. It houses and neighbors the esophagus, heart, and stomach. These organs are in constant motion and crave stability to counterbalance the tendency to be mobile. The left lower lateral ribs will be position in an out flared posture.
The left lung is more mobile and expressive than the right lung. It houses and neighbors the esophagus, heart, and stomach. These organs are in constant motion and crave stability to counterbalance the tendency to be mobile. The left lower lateral ribs will be position in an out flared posture.
Our feet’s ability to connect to the ground helps build foundational stability to the lung and diaphragm from the bottom up’s perspective. The frequent presentation will be someone that favors standing on their right leg to ground the right lung, but it is the left lung that requires more stability.
The suggested exercise called the “Standing supported left glute push technique” has one biasing loading the left leg and hip while reaching with the left arm forward and slightly downwards. This position will close the left rib into the exhalation posture. You are emphasizing the left side to feel that extra-connection from the ground up so it can rebalance the tendency of the left lung to be mobile and right lung to be restrictive.
Week 4 – Regulating Lung Carbon Dioxide (Capnia) Through Postural End Range Deep Breathing.
This week’s webinar talks about the concept of respiratory acidosis and alkalosis, with the right lung favoring the former, and left lung biasing the latter. The right lung’s tendency to be in respiratory acidosis, or synonymously with the word HYPERcapnia or HYPOventilated respiratory pattern, places the left lung to be in a HYPOcapnia state or hyperventilated pattern.
This idea piggy-backs off of last week’s webinar about the connection of the lungs with our feet. The right lung tends to be restrictive. The right lung is overly supported with a right leg stance and underlying visceral organ of the liver. This restrictive pattern of the right chest wall causes an inadequate exchange between the carbon dioxide (CO2) from the body and the oxygen (O2) from the air. You get too much CO2 and not enough O2.
A list of symptoms of respiratory acidosis includes shallow breathing, fatigue, possible disorientation, and headache from lack of oxygen.
A practitioner should be aware that narcotics, sleep medications, and central nervous system disorder tends to facilitate the combination of right lung restriction pattern and hypercapnia state.
Over time, the left lung will compensate with the out flare rib posturing. This was the topic for last week’s webinar. The result will the hyperventilated, or hypocapnia and hypocarbia state. The left lung will be lacking sufficient CO2 and holding too much oxygen in the lung and bloodstream. This idea may sound good, but you need carbon dioxide to bring oxygen into our cells and muscles for strength and movement.
The treatment of choice is called the “Wall Supported Squat with Balloon” You are focusing on loading the left leg and rib cage. The subtle weight shift to the left will reposition the diaphragm’s central tendon to be over the left hip for stability that the left lung craves. The slow inhale, and exhalation will stimulate the chemoreceptors to rebalance the respiratory pH load to the lungs and bloodstream. The tucked pelvis and spine, with the reaching of the right arm, will stimulate the mechanoreceptors to open up the restriction to the right lateral and anterior chest wall. It is common to get a relaxation effect due to the stimulation of the left nasal parasympathetic system. This further will help normalize your physiological system with bronchodilation.
Week 5 – Managing Chronic Obstructive Lung Dysfunction.
This week’s webinar talked about the undermanaged and “more common than you think” subclinical obstruction of the lung that does not allow you to get optimal gas exchange and rotatory movement. The webinar introduced respiratory numbers such as listed below.
- Forced Vital Capacity (FVC). The amount of air exhaled through force after the deepest breath possible.
- Total Lung Capacity (TLC).
- Residual Volume (RV).
- Forced Expiratory Volume (FEV).
You can quantify your progress and your air exchange, which is helpful for many people to know that every exercise will have a maximal impact. The reason is that when you get good ventilation to perfusion ratio and keep dead air spaces to a minimum, you will have great energy at your physical leisure! Another reason to measure expiratory volume is that many have no respiratory symptoms of shortness of breath and still have subclinical obstruction.
Obvious obstructive diseases include asthma and COPD, chronic obstructive pulmonary diseases like emphysema. We will talk about obstructive is similar to the restrictive lung. Diseases of restrictive diseases include pulmonary fibrosis or sarcoidosis.
These respiratory numbers help to detect subclinical obstruction. The pattern is that when you are obstructed, you will have an inability to expel air out of your lungs. You will have more residual volume due to a persistent state of hyperinflation. You get air in, but the obstruction is limiting the carbon dioxide release.
If you follow last week’s notes, the obstructed lung tends to be the LEFT lung. The side that begins as HYPERventilated and HYPOcapnia lung. The less stable side with a flared out rib. Your body will be positioned with a shift towards the right, shoulders dipped to the right, and head cocked the other direction.

When you treat and shift the pattern to un-obstructed, you will get less “left-over” gas in your lung. This will alter respiratory pH and ventilation to perfusion ratio. Your body will rebalance the other lung when you focus on one side and do it well. Can you see how the past webinars are tying together?
Next week’s webinar is on the role of the abdominals muscle, which plays a role in positioning your rib cage and allowing good fulcrum for diaphragm’s central tendon function at rest. If you noticed, most of the prior exercises focused on getting good natural abdominal contraction to alter rib positions and lung physiological function.
How or why would you get a minor obstruction in the first place?
- The lateral ribcage will look is altered because of improper abdominal to diaphragm recruitment.
- Your abdominals are relaxed and “quiet”, which allows you to not flex and fix your lower trunk for efficient respiratory and core control. You arch and extend your spine with more psoas and paravertebral activity at early INSPIRE.
- Your neck muscles and accessory muscles will over-activate to help push air out during EXPIRATION since there is resistance from the obstruction. (Increase Functional RC meaning it takes more volume for you to have ZERO airflows. This occurs when your rib cage elastic fibers cannot stretch out, or expand because the lung’s elastic tissues are tugging in the opposite direction with deflating.
- This all leads to hyperinflation. (more oxygen in the blood and less CO2).
- Loss of proper diaphragm function around the costal region resulting in the ribs to stick up and outwards. Again, this is reinforced by the psoas and paravertebral muscles.
- A forward head posture will shift the anatomy of the upper airway to be more susceptible to collapse and obstruct the air exchange even further.
The summary is that a weaker abdominal to diaphragm interaction will reposition the rib cage and spine to be in a vulnerable, unstable, weaker, and resultant, lower obstructive airway. The pattern is reinforced with a hypertonic psoas and spinal paravertebral muscles. Your neck and accessory muscles will have to work harder and impact expiration volume.
The exercise for this week is Standing Wall and Chair Supported Reach and Reverse Squatting. They both piggy-back the past’s webinars and bring forth the importance of leveraging your reaching and planting your feet firmly to the ground, to engage your abdominals. This will bring an end range rib cage position that will realign and rebalance any malposition that is obstructing your airway.
We will continue to bring cliff-notes to the next few webinars from Postural Restoration Institute’s COVID-19 webinar. This has been fascinating to listen and reinforces the importance of understanding how anatomy, physiology, and sound biomechanics can help you to heal and be active.
The webinar’s highlights PRI’s philosophy and it allows us to have another perspective when it comes to the numerous of clients we see with pulmonary trauma, respiratory symptoms as an underlying root cause for their pain, and the classic posturing we wrote about earlier.
As we are asymmetrical creatures that have asymmetry habits at work and in life, these suggested exercises will help us regain the balance and alignment that will sustain our physical and mental well-being.
If you need an expertise to evaluate any stubborn muscle or joint tension or pain, click the orange button to get your free phone consultation or telehealth consultation with Dr Ngo. You will get a sense of what is holding you back and general guidance on what is your next best step to recovery.
We specialize in recurrent muscle tightness and the pain the comes with it. Get your expertise second opinion with a click of the orange button below.
One LOVE,
Danh Ngo PT, DPT, OCS, SCS
Doctor of Physical Therapy
Board Certified Specialist in Orthopedic and Sports Medicine
Certified Advanced Movement Specialist – RockTape
Mind Body Health Results Coach





