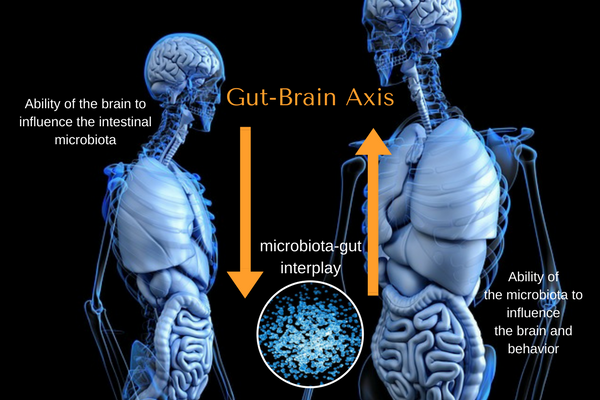
Gut and Brain are not separate. The National Institutes of Health, or NIH, in 2007 decided to start The Human Microbiome Project to help us learn more about this connection, called the gut-brain axis. President Obama realized the importance of our gut microbiome to important diseases such as Alziehmers, Parkinson’s, depression, autism, chronic pain, thyroid dysfunction, and cancer, that on May 13,
The first place to begin explaining about the gut-brain axis is called the Enteric Nervous System (ENS) is referred to as the 2nd brain. The ENS is made up of 50-100 million nerve cells. There are as many nerve cells in your gut as in your spinal cord! Your gut can work without your brain due to your Enteric Nervous System. Michael
The second place that connects your gut to your brain is called your gut microbiota. Your gut microbiota is an ecosystem that consists of 1,000+ bacterial species. The gut microbiota is designed to help us to thrive and contain more than 7,000,000 genes! This number indicates that we have more gut bacteria genes than the genes that make up our human genomes. The gut microbiota consists of viruses, fungi, and archaea too.
The research is showing that your unique gut microbiota is dependent on your human genes, your mother’s microbiota, your family’s microbes, your diet, and your brain’s activity and state of mind! Yes, your mood tendencies and how you feel pain are impacted by your gut! The other way goes in that how you hold your emotions can slow or speed up your digestion! This is one reason why we preach to “never chase pain or mood”. Visceral manipulation helps us to directly work on your gut mechanics to help you feel better overall.

There are immune system cells in your gut make up the largest part of your body’s immune system. Cytokines are produced by these immune cells to help defend you from getting sick. The gut-based immune defense system is designed to kill a single species of dangerous bacterial invaders that infiltrate your digestive system when we accidentally ingest something “bad” like contaminated food or water. The foreign invader is detected in an ocean of 1,000,000,000+ of beneficial microbes living in your gut microbiota.
So far, you have read that the gut is more than stomach, intestines and colon. Your gut has its own network of nerves and neurons. Your gut has its own immune system. There are a diverse groups of “outsiders” called the gut microbiota or gut microbiome that exists in your gut. You have a mutual relationship where you help them and they help you.
A crucial role of your gut is its ability as a sensory organ.
Your ENS, enteric nervous system, handles about 90% of what your gut cells sense. If you imagine the role of your skin cells is to help you to feel the world around you. Your gut has more “sensory” cells than the size of the surface of a BASKETBALL COURT. We only think of our gut as an organ to help us taste. You can see how the gut is still a big mystery to medical scientists currently. What the ENS senses never reaches your conscious awareness. Your ENS functions behind the scene and is finally getting the recognition it needs as.
The gut’s numerous sensors within the lining of the gut surveys and communicate with the enteric nervous system (ENS) on how to act and what is happening. The ENS gets information to help it learn and modify the intensity of peristalsis, direction of where the food should go, identify the presence of “bad” invaders and toxins, and production of enzymes and digestive aids.
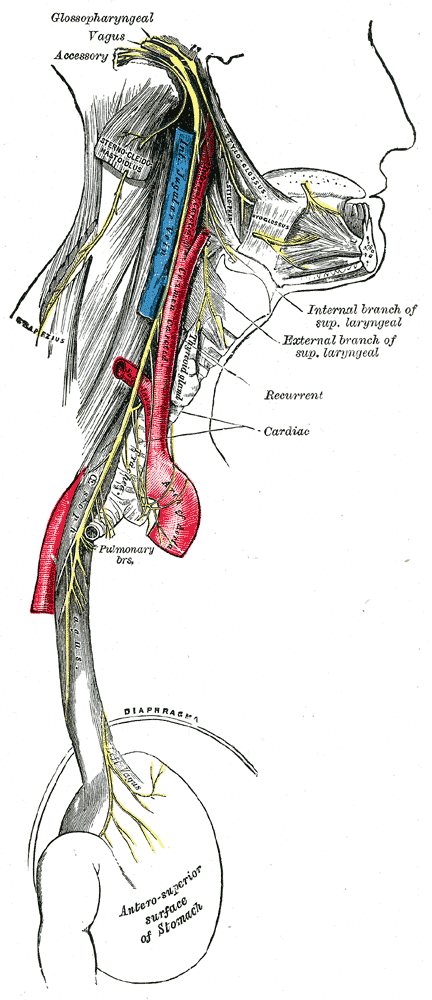
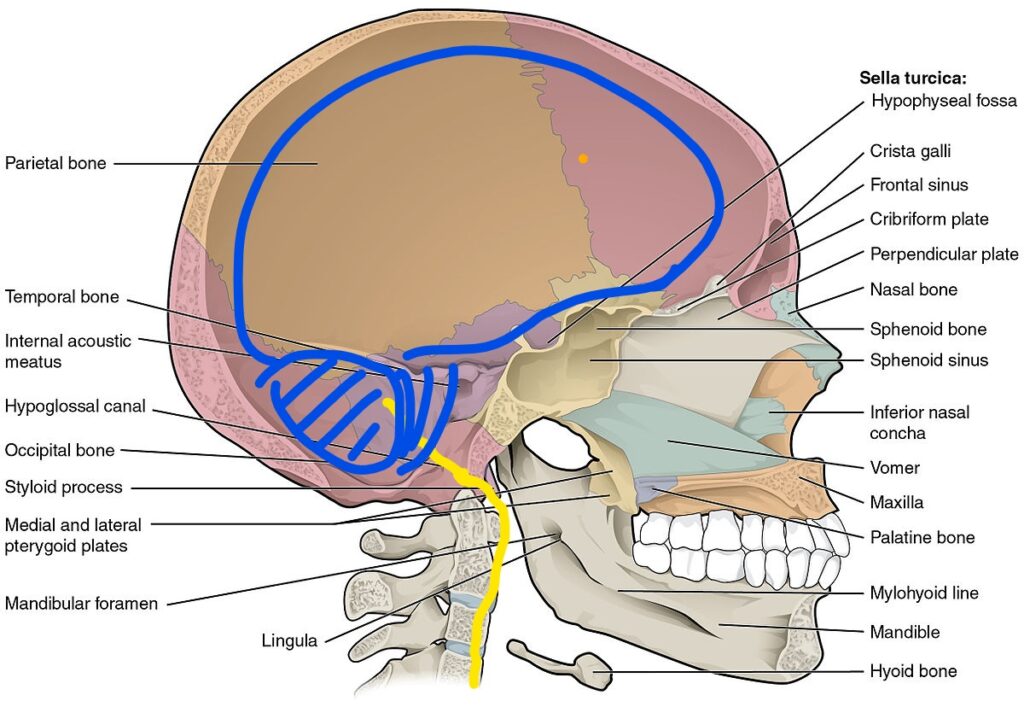
Where is your true brain, the cerebral cortex, in all of this? The gut tells the brain 90% of what is happening via the vagus nerve. In the picture shown, the vagus nerve is shown as the yellow line.
The food you eat cause a reaction. When you eat food, the gut bacteria, virus and fungi take on this food information based on the bacteria’s genes to produce 100+’s of by-products or metabolites that talk to the local gut cells or travel far to another location within your body. The local gut cells include the cells that impact your digestion, immune, and endocrine. The bacterial metabolites travel via the bloodstream as gut hormones (also known as gut peptides) or vagus nerve to the brain to produce a reaction.
Everyone has a unique mixture and diversity of gut bacteria. The bacteria and its genes make you digest, feel and act differently than your family member or friends. This is why everyone has a different combination of food sensitivities and the symptoms it produces.
A juicy strawberry will be broken down and produce a metabolite molecule based on the bacteria’s genes instructions to the bacteria. This molecule will float in your bloodstream to react to your brain differently than your friend would. The strawberry molecule can react to your digestive nerves to give you diarrhea, while your friends get constipated, based on your bacteria’s genes.

There is current research that has demonstrated lab rats and horses living in germ-free environments have a negative effect on their brain development and health! Our gut microbiome is impacted by the food that we eat. You can change a diet which change your gut ecosystem in
As we talked about gut lining and sensory cells, your digestive system’s ability to communicate depends on receptor molecules located on ends of these gut nerves called sensory nerve endings. The receptor molecules are on the hormone-containing transducer cells. Receptors are protein molecule within a cell, whose job is to bind chemicals and communicate to the cell itself.
Why does receptors molecules or sensory nerve endings matter within the gut-brain axis and how you feel?
The gut microbiota figures out what you are eating and produces the metabolite chemicals. Receptors senses and binds to the chemicals that are a great fit to it. Chemical competes with these receptors. A reaction occurs based on which chemical wins the battle of getting the receptors attention.
An example is when you eat an apple, the chemical of the apple is bound to the receptors of the taste bud cells. Your taste bud cells talk to your brain and lets you know that you are eating an apple. Surprisingly, your gut lining is filled with receptors with the same taste job duties of your tongue’s taste buds. Current research has shown that mouse intestines have at least 28 phytochemical receptors (receptors that recognize specific chemicals in plants).

There is a saying that your gut has a twin or mirror cell of what your brain contains. Your brain and gut have cells to help you taste. Your gut has smell receptors too. The purpose of these taste receptors in the gut helps your body to know what and how to breakdown your food. Receptors for sweet foods release insulin in your pancreas, absorb glucose into the bloodstream and tell our brain that you are full. Bitter taste receptors produce the hunger hormone called ghrelin. You can see how your gut plays a big role in the saying “taking in the experiences”.
At this point, you understand the gut-brain axis and how it communicates. The gut has multiple layers. The layer that gets in contact with the food you eat will be the outer layer. The inner layer will be considered the other side of the outer
The nerve cells called neurons are located on the inside, or the other side, of the gut lining to be protected from the harsh chemicals and gut microbiome. Your gut nerve cells rely upon the endocrine cells, like the earlier mentioned serotonin-releasing or hunger hormone ghrelin, to know which way it should act. To be clear, if you feel hungry, ghrelin can stimulate the nerve cells within the gut lining to tell the brain that you are hungry via the vagus nerve pathway. The hormone ghrelin can also travel within your bloodstream to your brain.
Your immune system cells within your gut work similar to your nerves in that the cells are separated from your gut lining. The inflammatory cells consist of cells in your small intestines called the Peyer’s Patches, appendix, and the cells in the wall of the large intestines. These inflammatory cells make cytokines. The inflammatory cytokines can cross into the bloodstream to talk to your brain.
There are special immune cells called dendritic cells. The dendritic cells branches and can access the gut outer layer’s environment, including the gut microbiome and harsh chemicals.

Why have two brains for digestion?
Your big brain’s role is to act only when necessary. Dr. Emeran Mayer’s theatre analogy answers this question well. He says that our brain is the producer. Your brain oversees your gut, heart, lung, muscles, and the rest of your body, with a priority of keeping you safe and well. The director is your gut. The director’s role is to understand the cast and crews and to make sure production goes well. If there is a disgruntled actor, the director needs to act accordingly. The brain or producer steps in when the disgruntled actor goes ballistic and the film is in jeopardy. The producer takes in information from every important staff and makes decisions accordingly. This intake of information is called “Interoceptive” information.
How did we get this gut-brain axis design in the first place?
The gut-brain axis can be found 500 million years ago. Gut scientists are using a new terminology called “microbe-speak” to also explain the gut-brain axis. As we describe above, microbe-speak is the way your gut microbiome communicate directly to your ENS, the second brain, and indirectly to your big brain. Biologists have found out that this fascinating process of microbiome speaking as being present 500 million years ago!
There is a small marine animal called the hydra that has a simple version of having a digestive system filled with microbes. The hydra is a few millimeters long! If it digests something bad, it spits it up just like how you vomit after eating something bad! The beginning of this gut structure and function advanced to having the enteric nervous system. The hydra is still present in fresh water today.
As we mentioned earlier, the gut microbiome functions as part of this dialogue of food, digestion, and bodily response, such as pain, mood, and overall well-being. The majority of the microbiome helps us do things our gut cannot do. It protects us and lets our immune system defend us from getting really sick. Your microbiome food consists of food our body can not breakdown, like dietary fibers and complex sugar molecules.
The group of foods that is important to eat and a food source for our gut bacteria is called pre-biotics. The prebiotics and dietary fibers are consumed and give us extra calories for us to survive during starvation times. The extra calories cause us to gain weight in this modern world, but an important part of gut health. We are advancing in the modern world too fast that we are having trouble understanding how to balance and respect this “ancient binding contract” that
There are harmful microbes called pathobionts that trouble our gut-brain axis. If our immune system is weakened, the pathobionts come out from hiding in the diverse neighborhood of good bacterias, viruses, and fungi. Pathobionts can use their molecular tools to attack your gut lining to cause inflammation and gut to “leak” into your bloodstream. This will result in your immune-system being on high alert as there are foreign substances in your bloodstream. The foreign intruders can travel and cross your blood-brain defense system to impact your brain health and function.
Pathobionts are caused by modern-society problems of relying on the SAD, standard American diet of unhealthy oils and reliance on intense artificial flavor enhancement, antibiotics, lack of good stress management strategies, environmental toxins, and less reliance on natural sources of healing. Environmental toxins come in the form of pesticides, herbicides, chemicals used in the ’50-’80s that infiltrated our soils, air fresheners, cleaners, fluorescent lights, and air pollutants. Natural methods of healing that we don’t use enough of include “undistracted and pure” social connection, grounding, sunlight, and spending more time with nature’s water and forestry.
As a quick recap, your gut has its own brain. The enteric nervous system has nerve cells that sense what is going on. The ENS uses the gut microbiota to help it understand what you are eating and how your gut should respond. Digest? Vomit or diarrhea? Constipation? Your gut has immune system cells that help to make sure you are healthy, based on what your ENS and gut microbiota decides is best for you. The microbiome is disrupted with “invaders”, or called
As we talk about your gut nerves, there is an important nerve, that we briefly mentioned earlier, that connects your brain to your digestive system. The nerve is called your 10th cranial nerve, or often named your vagus nerve. Your vagus nerve helps to communicate about 90% of what is happening in your gut to your brain. Your brain tells your gut 10% of what it needs to be doing through the vagus nerve. To quickly summarize an important concept: your brain relies on your gut to give it information, while your gut does not need your brain to act. See our article on the vagus nerve to see how common it is to have a dysfunction to your vagus nerve and whether treatment can help you. In the past, if doctors think you have a vagus nerve problem, they would cut the nerve and cause a whole range of problem that affects your lungs, heart, digestion, and more.
As an important side note, your vagus nerve starts from a part of your brainstem, called the medulla, and travels out the skull called the jugular foramen. The jugular foramen is a hole near the underside of your ear lobe. Two other cranial nerve comes out of there called your accessory and hypoglossal nerve. The area can be congested like your lower back can get pinched and cause sciatica. If you look at the picture, the nerve is close to your upper neck segments called the cervical vertebrae. If you look at yourself in front of the mirror and notice your chin is off-centered, then you can assume your first, and possibly your second vertebrae are positioned in a shorten hold.
In chiropractic philosophy, your vertebrae become subluxated and off alignment. We do not believe in this theory as no current research has validated a vertebra being
How does your gut work?
Your digestive system is amazing in its design. To make sure we are on the same page, your digestive system starts from your mouth to your rectum. If you think about the design, your gut, from your mouth to your rectum can be looked as separate from your inner body’s environment. Your gut is a continuum of the outside environment that is located within our body, which consists of bacteria, archaea, fungi, and viruses. Your gut has its own ecosystem like the Wakanda from the Marvel movie “The Black Panther” called the gut microbiota.
As we have talked about the role and importance of the gut, it is time to talk about how our intestine is coated with a mucus layer. The mucus layer is paper thin and is where the bacteria, virus, and fungi live. The mucus layer sits on the numerous sensors and specialized immune and endocrine cells that line your intestines. There is a gut condition called intestinal permeability dysfunction, fancy for “leaky gut“. The paper-thin lining of the gut develops bigger pores that allow your blood to be filled with unwanted materials, hence the simple name of “leaky gut”. Leaky gut is a common reason for having pain that does not go away easily. Read our article on this topic of Leaky Gut.
The lining of your gut plays a role in your hormone system, aka endocrine, as it contains up to 20 different hormones. The endocrine system is defined as glands that make hormones. The hormones can travel through our bloodstream to impact local or a location far distance from the gland. This is why the endocrine system affects the whole body. Your gut has more endocrine cells than all the other, more talked, about organs combined, including your gonads, thyroid gland, pituitary gland, and adrenal glands!
One important hormone that you may know in mood and well-being is called serotonin. A majority of your serotonin, about 90%, are stored in your gut. Serotonin is a molecule that signals to your body and brain to move food (intestinal function), tell you how much pain you are feeling (pain sensitivity), appetite, sleep, and is widely known as a key component within anti-depressants treatment.
Your gut plays a role in your mood and pain. Serotonin is one reason in your gut-pain relationship. We have a saying here at ReVITALize Rehab Club that goes “Never chase your pain or mood”.
To quickly summarize (in
WHEN GUT GOES WRONG.
If a healthy gut-brain axis is dependant on your the bacteria, virus, fungi and archea within your gut microbiome, a disruption of this microbiome is called gut dysbiosis.
As we are learning from the research and the Functional Medicine perspectives, a stool sample is can help us learn more about your gut microbiome. The tricky aspect of interpretating the data is that there is very conclusive research that indicates what is “bad” pathogens.
For example, candida is a popular blame in the past decade over the internet as a source of bad fungi and yeast. Candida is normal to be found in your gut microbiome. The problem happens when your immune system and over-all mind-body is weaker, then the candida becomes a bully. A person maybe considered a bully based on the resilency of the physical and emotional make-up of the individual that is experiencing the bullying. V
How your emotions and gut are connected.
Emotions produce a predictable response to our upper and lower GI tract. The predictable response is led by two main factors. The hormones and nerves that connects between the brain and gut systems. The individual intensity and demonstration of our emotions are based on how we interpret a situation. We watch a sad movie scene that makes us feel sad. It makes us feel empathy, cry or subtly not sit as tall to acknowledge an understanding that it is a sad situation.
As we go back to Dr.Emeran Mayer MD’s book the “

The opposite response of having an underactive upper and lower GI happens with the emotion of sadness. The food that you ate does not get digested well with the right mixture of stomach acid and enzymes. The poorly digested food can stay longer in your gut and ferments with bigger food particles hanging out. Your gut good versus bad bacteria, fungi, and viruses can shift towards dysfunctional state called gut dysbiosis. Your large intestines may not absorb enough water so your poop is looser than usual.
In the case of the feeling of fear, your stomach (upper GI) becomes underactive by not producing enough stomach acid, and your lower GI (intestines) becomes overactive by producing enzymes to breakdown food and over absorb water so you become constipated.
As we are learning more about Functional Medicine, you cannot get a lasting solution to a gut problem without acknowledging the importance of the mind. If there is a strong emotional trigger or earlier emotional trauma, this can lead to a poor gut, pain, hormonal, or athletic performance. There is numerous strong evidence that a brain-gut axis dysfunction is a source of irritable bowel syndrome, chronic constipation, indigestion, and functional heartburn.
Your brain-gut axis is heavily impacted by physical or emotional stress. The intensity of the response is based on our interpretation and reaction to stress. Our brain consists of conscious and subconscious brain. The hypothalamus is part of the subconscious brain that releases a molecule called CRF, cortico-tropin releasing factor. This acts as a master switch that turns on every vital organ systems to emergency protective mode. Full-blown or chronic symptoms occur when we reach our limits, known as our physical and emotionally trained-capacity. Cortico-tropin releasing factor (CRF) releases hormones called cortisol and norepinephrine.
Jaak
Since this is not an article on genes, we will keep the information short to the idea that genes are given by our parents, but turned on and expressed by what we experience throughout our life. The common on-switch that is
A neuro-tag and a chemical tag is a file of an experience. The experience includes a report summary of your senses: sight, hear, touch, smell, taste, and thought. The body and brain quickly have to tag what you are sensing to help you short-cut any similar experiences in the future. The tricky part is when you experience a sight or feel anything that is similar to what is filed as a neuro-tag or chemical tag, your body and brain will theater and showcase everything that comes within this file.
An example is if you got into a heated argument with a friend while you were eating at a restaurant. During this moment, you heard the chef press a bell to let the waiter know that the food is ready. You hear the “ding” as you smell the aroma of a grilled patty. The neuro-tag and the chemical tag is storing the emotion of feeling angry, the smell of a juicy grilled beef patty and the sound of the bell.
There is a saying that goes “nerves that work together, fires together”. Two factors
Your body and brain will pull that whole file, neuro-tag and chemical tag, to help you act faster. Your heart rate increases, your gut’s upper and lower system become over-active, and starts over-production of enzymes, stomach acid and absorb more water within your large intestine. You become constipated. This is actually a protective response. If you were hunting or being hunted in the past, you have to make quick decisions to stay alive.
Each of the emotional operating system (EOS) in the brain uses a specific molecule to talk to the body and gut. When the chemical molecule is
As many know the hormone serotonin as a molecule that helps us feel happiness, it plays a role in modulating cognition, memory, reward, learning, and numerous digestive functions. Enterochromaffin cells release serotonin when the upper gut is moved by mechanical shearing forces of food sliding and rubbing against these cells. The enterochromaffin cells help with peristatsis reflex, but a strong dose leads to vomiting or bowel movement. There is research that shows if you lower your diet in tryptophan, an amino acid needed to make serotonin, can make you more sensitive to having depression and an increase sensitivity to mechanical stimulation of the colon.
As we mentioned on how 90% of serotonin is stored in your gut, the vagus nerve pathways are located close by. If you are constantly eating, the mechanical stimulation rubs and excite the vagus nerve to tell the brain to make you feel good and well. The other batches of serotonin within the gut nerves also impact gut function such as peristalsis reflex. The remaining small patches of serotonin are in the brain, which functions in other serotonin’s duties in how you feel pain, appetite, movement, and mood.
Gut peptides (also known as gut hormones due to its ability to travel in the bloodstream) play an important role
As a quick summary of how the brain and gut talk to each other, there are two main methods: long travel methods using peptides or hormones via the bloodstream and through the nervous system. Hormones use receptors as a way to know when to shut down or become activated. Chemical signals can either be inhibitory (shuts down or dampens) or excitation (turns on or amplify) of a bodily reaction like digest faster or slower. Your gut has nerves within the Enteric Nervous System (ENS) that senses and respond. There is a big traveling nerve called the vagus nerve (cranial nerve 10). The vagus nerve comes from the big brain and controls the rest and digest response, or parasympathetic phenomenon.
The enteric nervous system is the second brain and its role is to maintain gut function and relay the information about how food and what you are sensing impacts mood, decisions, how you feel pain, how you handle inflammation and toxins, and the obvious, gut functions. Our gut microbiome, a diversity of bacteria, fungi, archaea, and viruses, works very closely with the ENS. Your ENS collects the gut report from the gut microbiome to know if it should protect or not, thus causing you to vomit, have diarrhea, constipation, or other gut reaction. This is called “microbe speaks” or gut-brain axis.
If you would like to understand more about your gut health and its role in your symptoms of pain or mood, reach out to us by clicking on the button below. There is no commitment as you will be having a chat with

As we wrap up this article, we would like to emphasize that you can get better once you tap into the body’s holistic healing power and use clear lab data to guide you step by step towards recovery using a Functional Medicine’s perspective.
One LOVE,
Dr Danh Ngo
Board Certified Orthopedic and Sports Medicine Specialist
Doctor in Physical Therapy
ADAPT Functional Medicine graduate class of 2020.
